By Elizabeth Anderson, LCSW, DSW and Dale Lupu, MPH, PhD
When I was first told I had chronic kidney disease (CKD), I was grateful that there were lifesaving treatments, but I was also scared because I didn’t have a plan. I worried that I might be in pain or become a burden to my family. I felt better when I was able to discuss my desires and healthcare decisions with my family and healthcare team.
What kind of medical care would you want if you were too ill to express your wishes? Like most people, you may not have thought about it, or you may have a difficult time discussing it with your family and kidney care team. However, planning for your healthcare in the event that you cannot speak for yourself may help decrease your worries. This process is called advance care planning.
Some people know exactly what they would want to happen if they became very ill. For other people, these decisions take time and thought. It helps to talk to a friend or family member and to ask your kidney care team to help you make a plan and put it in writing.
The Coalition for Supportive Care for Kidney Patients has outlined five steps to help you with your advance care planning:
- Choose someone to make healthcare decisions for you if you get sick and cannot speak for yourself.
- Think about what kind of healthcare you would want if you were unlikely to get better. Discuss your wishes with your family and friends.
- Write your wishes down in a legal form, known as an advance directive (sometimes called a “living will” or a medical power of attorney).
- Give a copy of your advance directive to your healthcare agent and your kidney care team. Continue talking to your family about your wishes.
- Discuss with your kidney care team when a medical order form (usually called POLST or MOLST) might be right for you.
The guide from the Coalition’s project called Make Your Wishes About You (My Way) is available for free. (http://go.gwu.edu/MyWayACP). The My Way guide is written especially for patients with kidney disease. It guides patients through the steps of advance care planning and gives helpful worksheets and tips.
You can begin to work on each of the five steps for advance care planning by following these detailed instructions from the My Way patient guide:
STEP 1: Who is your healthcare agent?
Choose someone—such as a trusted family member or friend—to act as your healthcare agent. This person will make healthcare decisions for you if you get sick and cannot speak for yourself.
- A healthcare agent has no authority in your healthcare unless you are unable to make decisions for yourself.
- A healthcare agent has no power over any other part of your life (e.g., finances, will, etc.).
- If you do not have a healthcare agent, then your kidney care team will usually ask your next of kin.
- A healthcare agent is only official if you complete an advance directive. Be sure to share the advance directive with family and your kidney care team so they know who to turn to if needed.
STEP 2: What would you want people to know if you got sick and were not able to speak for yourself?
Think about what kind of healthcare you would want if you were unlikely to get better. If you got so sick that you could no longer do most of your daily activities, or if you were near the end of your life, what would you prefer to be the focus of your care?
- Staying alive at all costs, no matter the pain or discomfort involved.
- Being as comfortable as possible, even if it meant you might not live as long.
- Not sure or it depends on the situation.
Each person has a different view of what they would want at the end of life based on his or her personal values and current health status. Talk to your kidney care team to learn more about the risks and benefits of different treatments for you.
STEP 3: How do I make my medical wishes known?
Write your wishes down in a form called an advance directive (sometimes called a “living will” or a medical power of attorney). Your kidney care team can help.
- An advance directive is a legal document that allows you to have control of your healthcare decisions if you are ever unable to speak for yourself.
- Use the form that is recognized in the state where you live. Two sites that have free forms for each state:
- Prepare For your Care: (https://prepareforyourcare.org/advance-directive)
- Caring info (https://www.nhpco.org/advancedirective/).
- Share the completed form with your healthcare agent, family members, friends, and kidney care team.
- Advance directives can be changed any time. Simply destroy the old document and create and date a new one.
Advance directives should be reviewed throughout a person’s entire life, especially:
- Before each annual exam
- After any major life change (birth, marriage, divorce, remarriage)
- After any major medical change, such as diagnosis of chronic kidney disease or hospitalization
- After losing the ability to live independently
STEP 4: How do I start the conversation?
Talk to your family and friends about the care you would want. Give a copy of your advance directive to them and your kidney care team. Avoid family conflict in a health crisis by talking about your wishes ahead of time. Ask family members to reflect on someone else’s experience with chronic illness.
- If you are part of a spiritual community, talk to your spiritual leader for guidance.
- Ask your kidney care team to help you find a social worker. They will have ideas about how to start conversations. Social workers can give you resources and get documents you need.
STEP 5: Discuss with your kidney care team when a medical order form (called POLST or MOLST) might be right for you.
POLST stands for “Physician Orders for Life-Sustaining Treatment,” and MOLST stands for “Medical Orders for Life-Sustaining Treatment.” The POLST form is a portable medical order form that records a patient’s treatment wishes so that emergency personnel know what treatments the patient wants in the event of a medical emergency. It helps individuals with serious illness or frailty to communicate their treatment decisions. The POLST form may be especially helpful if you are at risk for unexpected hospitalization or transfer to a different care setting. POLST is known by different names in different states; for a list of names, visit www.polst.org/programs-in-your-state.
Action Items
- Think about what you want your future medical care to be like.
- Seek input from your family, kidney care team, and/or spiritual leader.
- Tell your family and friends your wishes.
- Formally ask someone you trust to be your healthcare agent.
- Fill out an advance directive, naming a healthcare agent.
- Provide copies of your advance directive to your kidney care team and other doctors.
- Provide copies of your advance directive to your healthcare agent.
- Ask your kidney care team to record your wishes as medical orders, often called POLST or MOLST.
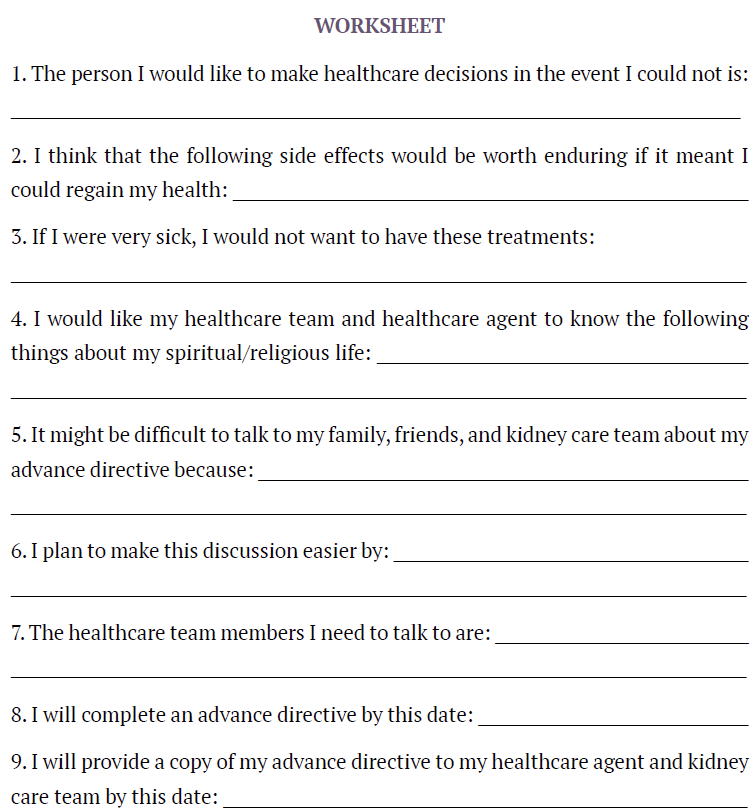
If you need additional help in reflecting on your healthcare wishes and goals, this worksheet from the My Way Patient Guide may help you.
Additional Resources
- The Coalition for Supportive Care of Kidney Patients’ website has many resources about advance care planning for people with kidney disease: https://www.kidneysupportivecare.org
- Prepare for your Care is a website with a step by step program, including video stories, to help with advance care planning: https://prepareforyourcare.org/welcome
- Prepare for your Care also has easy-to-read advance directive documents for every state and in several languages: https://prepareforyourcare.org/advance-directive
- The Conversation Project helps people express their wishes for end-of-life care, saying the place these conversations should begin “is at the kitchen table—not in the intensive care unit”: https://theconversationproject.org/
Elizabeth Anderson, LCSW, DSW, is an Assistant Professor of Social Work at Western Carolina University.
Dale Lupu, MPH, PhD, is Associate Research Professor at George Washington University.