
By Jay Wish, MD
Anemia is defined as a lower-than-normal level of hemoglobin in the blood. Hemoglobin is the protein in red blood cells that carries oxygen to all tissues and allows those tissues to carry on their functions, including the creation of building blocks for energy. Hemoglobin is what makes red blood cells red, and this explains why people with low hemoglobin levels may appear pale. Hemoglobin levels less than 13 in men and less than 12 in women is considered anemia. Anemia is common in people with chronic kidney disease (CKD) and may have many causes. It is estimated that 15.4% of people with CKD (stages 1-5) have anemia, compared to 6.35% of people without CKD. The frequency of anemia increases with the stage of chronic kidney disease: around 10% in mild CKD (stages 1-2), around 20% in moderate CKD (stage 3), around 50% in severe CKD (stages 4-5), and around 90% in people undergoing dialysis. There are a number of reasons why people with CKD develop anemia.
The kidney is the major source of the hormone erythropoietin, or EPO. The kidney has cells that sense the amount of oxygen in the surrounding kidney tissue, which is the amount of oxygen delivered by the red blood cells minus the amount of oxygen which the kidney cells consume. If the hemoglobin level is low (anemia), the lungs are not able to absorb oxygen from the air, or the person is living at high altitude where the oxygen level in the air is low, the cells in a normal kidney will sense that low oxygen level in the surrounding kidney tissue and will respond by making EPO. EPO will travel to the bone marrow and lead to increased production of red blood cells, correcting the anemia or even making the hemoglobin level higher than normal to compensate for lung disease or living at high altitude. In a person with chronic kidney disease the production of EPO is lower than normal, primarily because of fewer EPO-making cells. However, the amount of oxygen in the kidney tissue might be normal because the diseased kidney is consuming lower amounts of oxygen, so the oxygen-sensing cells do not increase the production of EPO despite the presence of anemia.
The other major cause of anemia in people with CKD is iron deficiency. Iron is an essential component of hemoglobin and is what makes hemoglobin red. Think what happens when iron rusts – it turns red. People with chronic kidney disease may become iron deficient for a variety of reasons. A diet low in red meat (as is becoming increasingly popular) may provide insufficient amounts of iron to meet daily demands. The body has a number of mechanisms to prevent the over-absorption of iron from the diet since once iron is absorbed there is no physiologic way to get rid of it. Oral iron supplements containing ferrous iron must be oxidized by stomach acid to the ferric iron form, so any medication that decreases stomach acid production (proton pump inhibitors such as omeprazole, histamine-2 blockers such as famotidine) or food which neutralizes stomach acid may decrease the absorption of these iron supplements. The absorption of oral iron supplements by the small intestine is under the control of a hormone called hepcidin. Hepcidin is stimulated in the setting of inflammation or iron excess. Since CKD is often accompanied by inflammation, hepcidin levels are elevated and increase with advanced stages of CKD. The inflammation may be due to a variety of factors related to the kidney disease itself or to other conditions including diabetes, heart failure, the presence of a dialysis catheter, or poor oral hygiene. Hepcidin also traps iron that’s already in the body into storage sites and makes it unavailable to travel to the bone marrow to support the synthesis of hemoglobin. This is called functional iron deficiency and generally does not respond to iron supplements administered by mouth, as may absolute iron deficiency which the iron stores in the body are low. Oral iron supplements are often poorly tolerated due to upset stomach and/or constipation, leading to the need for supplemental iron to be administered intravenously (IV). IV iron administration is very common in in-center hemodialysis patients who can receive it through the hemodialysis blood circuit during the treatment. People with CKD not on dialysis or on home dialysis who need IV iron will come to an infusion center to receive the medication which is usually well-tolerated although there are rarely allergic reactions.
Other causes of anemia in patients with CKD include blood loss (particularly among in-center hemodialysis patients
due to blood remaining in the dialyzer circuit following rinse-back, frequent blood testing, or vascular access procedures), which may be compounded by abnormalities in the blood clotting system due to the kidney disease itself and/or medications. It’s known that the life span of red blood cells is less than normal in patient with CKD (reduced by as much as 50%). The accumulation of waste products in people with CKD may decrease red blood cell production even in the presence of normal amounts of EPO and iron.
The symptoms of anemia are variable. Every person with anemia does not experience the same symptoms at a given hemoglobin level and not every symptom that may be associated with anemia is necessarily due to anemia since many people have multiple diseases than can contribute to these symptoms. The most common symptoms of anemia are fatigue and lack of energy. Since the anemia of CKD tends to be gradual in onset as the kidney function declines, the person affected may adapt to the anemia both physiologically and psychologically so that the symptoms are less than had the hemoglobin fallen to the same level over a much shorter period of time. Most people with CKD do not develop symptoms of anemia until the hemoglobin level is less than 10, and many do not develop symptoms until the hemoglobin level is even lower. A study comparing symptoms among people with CKD with and without anemia, with which I was involved, (Kidney Medicine, 2022, volume 4, page 100439) showed that those with anemia had small but significant increases in symptoms, poorer physical well-being, poor social/family well-being, poorer functional well-being, and increased impairment in activity, work productivity, and work time missed due to health. However, it should be noted that those without anemia also had significant symptoms, well-being issues, and activity impairment related to their CKD, concomitant illnesses, and/or medications. Other symptoms that have been attributed to anemia include leg cramps, impaired sleep, and decreased libido. Studies designed to assess the effect of anemia correction in people with CKD (with synthetic forms of EPO) have been unsuccessful in consistently demonstrating a decrease in anemia-related symptoms while increasing the risk of cardiovascular complications such as vascular access thrombosis in patients on hemodialysis, heart attack, stroke, heart failure, and deep venous thrombosis/pulmonary embolism.
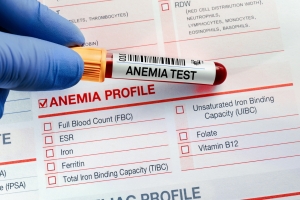 The international guidelines for the treatment of anemia of CKD recommend that all patients with CKD stage 3 or greater be tested at least annually for the presence of anemia with a complete blood count including hemoglobin level (more often in later stages of CKD or if anemia is present). If anemia is present, an evaluation for the cause of anemia should be undertaken with blood iron studies and possibly blood vitamin levels for folate and vitamin B12. If the person is iron deficient, evaluation for iron loss in the gastrointestinal tract may be appropriate. Treatment with an iron supplement can be by mouth or IV. Oral iron supplements may not be effective due to side effects which may limit adherence or to a severe degree of iron deficiency. Your provider might decide to go directly to an IV iron supplement, which may require several doses in an infusion center to provide a sufficient amount of iron to correct the deficiency. As noted above, people on in-center hemodialysis generally receive IV iron regularly through their blood circuit on the dialysis machine. If a person with CKD remains severely anemic (hemoglobin less than 10), then consideration is given to the use of synthetic form of EPO which is administered under the skin or IV. There are three forms of synthetic EPO currently available in the US: epoetin alfa (Epogen, Procrit or Retacrit), darbepoetin alfa (Aranesp), and pegylated epoetin beta (Mircera). They all have the same effectiveness in treating anemia and side effects, and their difference is in how often they are administered with epoetin alfa the most often and pegylated epoetin beta the least often. Your provider’s choice of a synthetic EPO drug will likely be determined by which form your insurance covers or which form is on the formulary of your dialysis provider. Because of the cardiovascular complications mentioned above associated with the use of the EPO drugs, the Food and Drug Administration (FDA) recommends that these agents be initiated only when the hemoglobin is less than 10 and that the dose be decreased or discontinued when the hemoglobin is greater than 10 in non-dialysis patients with CKD, and when the hemoglobin is greater than 11 in dialysis patients. The FDA does not acknowledge any quality-of-life benefit from these drugs, and views them only as a method to avoid blood transfusion. Blood transfusion is a last-resort treatment for anemia and is generally reserved for people with hemoglobin less than 7 or with sudden blood loss. The decision to prescribe a blood transfusion is made based on the severity of the anemia, the symptoms, the clinical setting, and rapidity of hemoglobin decrease. Blood transfusions may be associated with acute reactions, infections, and iron overload. More importantly for people with CKD, transfusions trigger the production of antibodies to human proteins, which may limit the options for future kidney transplantation from living or deceased donors.
The international guidelines for the treatment of anemia of CKD recommend that all patients with CKD stage 3 or greater be tested at least annually for the presence of anemia with a complete blood count including hemoglobin level (more often in later stages of CKD or if anemia is present). If anemia is present, an evaluation for the cause of anemia should be undertaken with blood iron studies and possibly blood vitamin levels for folate and vitamin B12. If the person is iron deficient, evaluation for iron loss in the gastrointestinal tract may be appropriate. Treatment with an iron supplement can be by mouth or IV. Oral iron supplements may not be effective due to side effects which may limit adherence or to a severe degree of iron deficiency. Your provider might decide to go directly to an IV iron supplement, which may require several doses in an infusion center to provide a sufficient amount of iron to correct the deficiency. As noted above, people on in-center hemodialysis generally receive IV iron regularly through their blood circuit on the dialysis machine. If a person with CKD remains severely anemic (hemoglobin less than 10), then consideration is given to the use of synthetic form of EPO which is administered under the skin or IV. There are three forms of synthetic EPO currently available in the US: epoetin alfa (Epogen, Procrit or Retacrit), darbepoetin alfa (Aranesp), and pegylated epoetin beta (Mircera). They all have the same effectiveness in treating anemia and side effects, and their difference is in how often they are administered with epoetin alfa the most often and pegylated epoetin beta the least often. Your provider’s choice of a synthetic EPO drug will likely be determined by which form your insurance covers or which form is on the formulary of your dialysis provider. Because of the cardiovascular complications mentioned above associated with the use of the EPO drugs, the Food and Drug Administration (FDA) recommends that these agents be initiated only when the hemoglobin is less than 10 and that the dose be decreased or discontinued when the hemoglobin is greater than 10 in non-dialysis patients with CKD, and when the hemoglobin is greater than 11 in dialysis patients. The FDA does not acknowledge any quality-of-life benefit from these drugs, and views them only as a method to avoid blood transfusion. Blood transfusion is a last-resort treatment for anemia and is generally reserved for people with hemoglobin less than 7 or with sudden blood loss. The decision to prescribe a blood transfusion is made based on the severity of the anemia, the symptoms, the clinical setting, and rapidity of hemoglobin decrease. Blood transfusions may be associated with acute reactions, infections, and iron overload. More importantly for people with CKD, transfusions trigger the production of antibodies to human proteins, which may limit the options for future kidney transplantation from living or deceased donors.
The treatment of anemia in people with CKD can be inconvenient for many patients not receiving in-center hemodialysis because it may require regular visits to a clinic or infusion center for the administration of EPO drugs or IV iron. There is a new class of anemia drugs currently under development, approved in other countries but not yet in the US, that is orally administered and may substitute for the EPO drugs. This class of drugs, called HIF (for hypoxia inducible factor) stabilizers, stimulate the EPO-producing cells in the kidneys and liver to make more EPO by making the oxygen sensors sense less oxygen. This allows people with CKD, even those on dialysis or whose kidneys have been removed, to make enough EPO to stimulate the bone marrow to produce more red blood cells and increase the hemoglobin level. There are three such agents which completed large scale global studies in people with CKD on dialysis and not on dialysis to demonstrate they are equally effective as EPO drugs in raising hemoglobin levels. The FDA did not approve two of these drugs due to safety concerns, but their manufacturers have the opportunity to do additional studies and request further review by the FDA for approval. The third HIF stabilizer drug is currently undergoing its first review by the FDA with a decision expected in early 2023.
In summary, anemia is common in people with CKD and is often associated with symptoms including fatigue, lack of energy, poor sense of well-being, sleep disturbances, leg cramps, and lack of libido. However, since many people with CKD also have other conditions and medications which may produce similar symptoms, it is often difficult to determine to what degree the anemia is contributing to their symptoms. Studies of anemia correction in people with CKD using EPO drugs failed to demonstrate a compelling improvement in anemia symptoms, while significant increases in cardiovascular complications occurred. The best approach to anemia in patients with CKD is early detection with regular screening for hemoglobin level, evaluation for iron and vitamin deficiency and blood loss. Iron deficiency is common in people with CKD due to dietary habits or prescriptions which restrict iron-rich foods, blood loss, and the adverse effects of inflammation on dietary iron absorption and release from internal stores. Iron supplementation, if needed can be oral or IV. If the person with CKD who is not iron deficient continues to have hemoglobin less than 10, consideration should be using an EPO drug, primarily avoid transfusion and not with expectation it will significantly improve symptoms.
Jay Wish, MD is Professor of Clinical Medicine at Indiana University School of Medicine and Chief Medical Officer for Out-Patient Dialysis at Indiana University Health in Indianapolis, IN. He has been in nephrology practice for over 40 years. He is particularly interested in anemia of chronic kidney disease and has written over 50 articles and book chapters on the subject.




