By Jackson Williams, Vice President of Public Policy, Dialysis Patient Citizens
Efforts to modernize the delivery of quality care to dialysis patients reach several milestones in 2020: Medicare’s first care coordination program for kidney care, the Comprehensive ESRD Care Model, expires at the end of this year; providers have been invited to participate in a new program, the Comprehensive Kidney Care Contracting Model; end-stage renal disease (ESRD) patients will, in October, for the first time have access to their choice of Medicare Advantage plans effective January 1, 2021; and a new bill is being introduced in Congress to create another integrated care option for kidney patients.
Why Care Coordination?
Most dialysis patients are served by “Original Medicare,” a program that attempted to duplicate health insurance as it existed in 1965. Under Original Medicare, each provider is paid on a “fee-for-service” basis, and no single entity is accountable for a patient’s overall health outcomes. For instance, hospitals, dialysis, and physicians generally provide care separately. Continuity of quality care can break down when there are transitions or handoffs from one setting or one provider to another. Few patients experience as many transitions as those with ESRD: from chronic kidney disease to dialysis, from dialysis to transplant, from hospitals to skilled nursing facilities or home, etc. In Original Medicare, there is no payment for activities by case managers, community health workers or “health coaches” who can try to keep patients from falling through the cracks during such transitions.
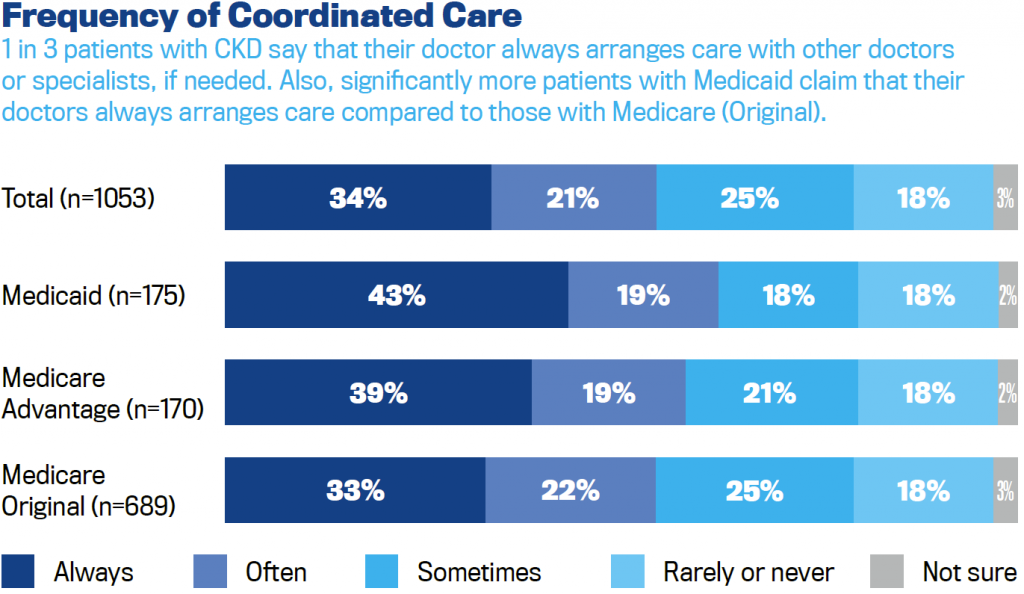
DPC’s 2019 Member Survey showed that a significant number of dialysis patients experience fragmented and disorganized care. Eighteen percent of patients say their regular doctor rarely or never helps coordinate or arrange care with other providers, such as specialists. Twenty-two percent of patients say that in the past two years they have had experiences where test results, medical records or reasons for referrals were not available at the time of a scheduled doctor’s appointment; doctors ordered a medical test the patient felt was unnecessary because the test had already been done; or doctors recommended treatment that they thought had little or no health benefit.
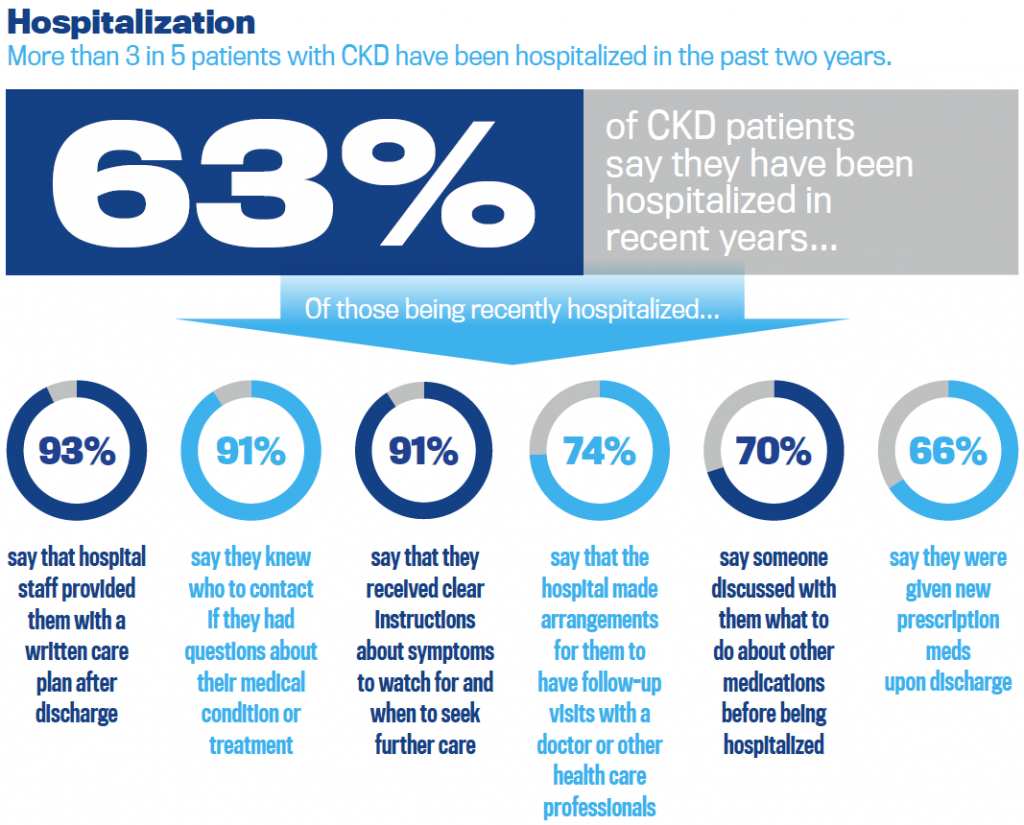
About a quarter of dialysis patients who’ve been hospitalized in the past two years say that the hospital made no arrangements for follow-up visits with a doctor after their discharge, nor discussed with them the medications they were using before their hospital stay.
Twenty-eight percent of dialysis patients say their doctor gave them instructions for one of their chronic conditions that conflicted with what they have been told to do for another condition, and that specialists they see did not seem aware of the different chronic conditions they had. These are substantially higher percentages than those patients with other chronic conditions have reported when asked the same questions.
A First Step Toward Integrated Care: The Comprehensive ESRD Care Model
Beginning in October 2015, Medicare’s Comprehensive ESRD Care Model established ESRD Seamless Care Organizations (ESCOs) for dialysis patients. ESCOs are formed by partnerships of dialysis providers and nephrologists. This is a pilot project, and Medicare permits ESCOs only in urbanized areas and adjacent counties, so their geographic reach is limited. There are 685 dialysis facilities owned by seven different providers, participating in ESCOs. That is 12 percent of clinics in the U.S., which includes 14 percent of Medicare beneficiaries with ESRD (about 72,000 patients).
The ESCO assumes responsibility for all the patient’s Medicare spending (except prescription drugs under Part D). If the ESCO keeps Medicare expenditures below average for an ESRD patient, it earns a bonus. This incentivizes the ESCO to coordinate care and do all it can to avoid complications and hospital stays. To prevent complications, the ESCOs deploy care teams that include nephrologists, nurse practitioners, case managers and pharmacists.
Overall, the ESCOs have been a success: Hospitalizations are down by six percent, and Medicare expenditures have been reduced by about $1,300 per patient each year. But not every individual ESCO has thrived: eight of the 37 ESCOs did not “beat” their benchmarks, so did not share in savings to Medicare. Also, because each ESCO must advance its own money to hire care teams, ESCOs that did not save enough money to cover that investment also finished in the red.
What’s Next for Care Coordination for Dialysis Patients?
Last summer, Medicare announced its intention to replace the Comprehensive ESRD Care Model with a Comprehensive Kidney Care Contracting Model. Details are still unclear, so it’s unknown how many ESCO sites will continue under the new program, nor whether additional patients will be served.
With the start of Medicare open enrollment in October, ESRD patients will for the first time have access to their choice of Medicare Advantage plans, effective in January of 2021. Medicare has not yet finalized rules for 2021 health plans, so it’s unknown what choices will become available nor how attractive they will be for dialysis patients. We do know that Medicare Advantage has served two categories of ESRD patients in the past: over-65 enrollees who had Medicare Advantage before their kidneys failed and members of a few “Special Needs Plans” exclusively serving dialysis patients. In these circumstances, Medicare Advantage plans have been effective in coordinating quality care.