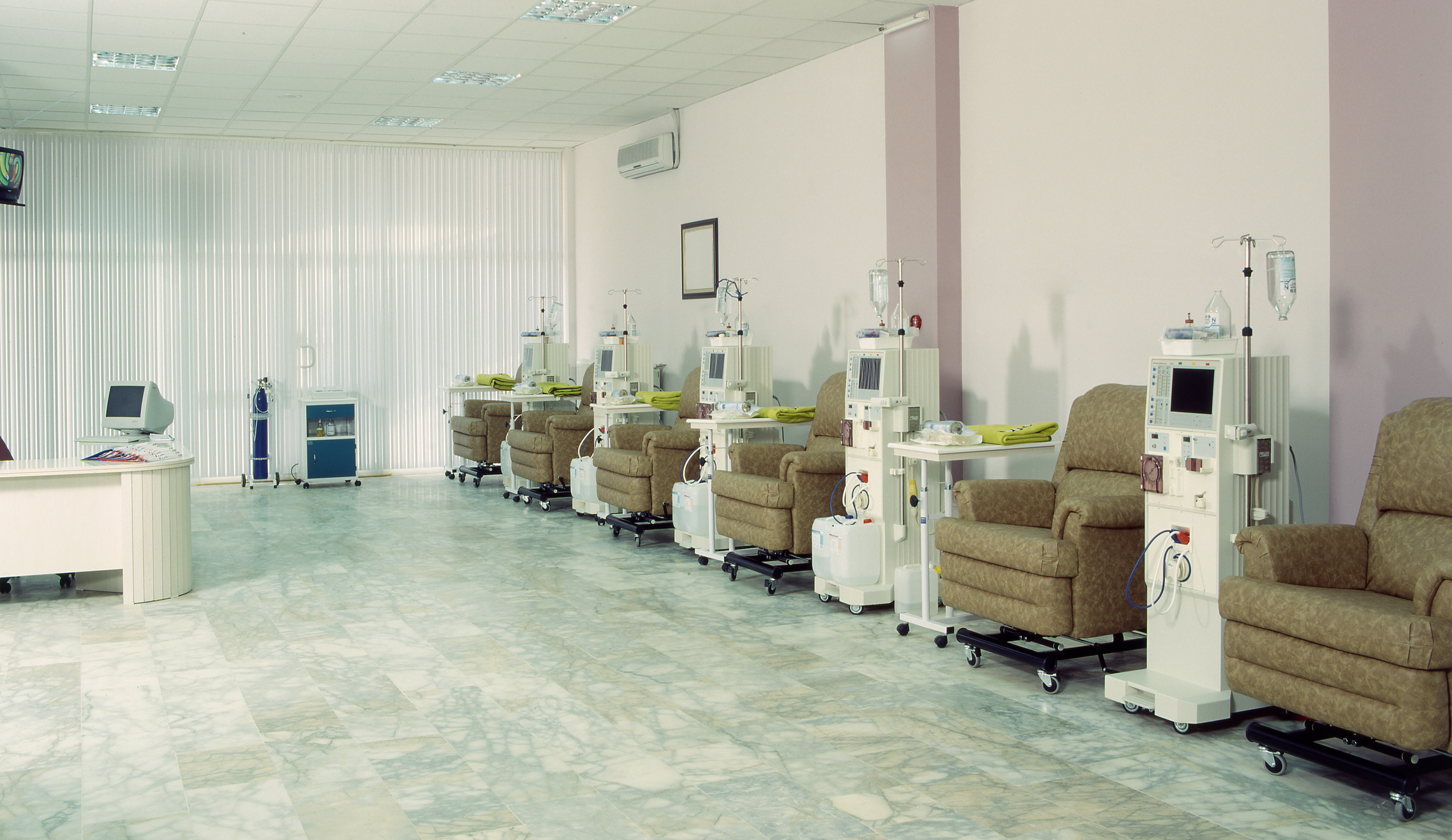
Currently, in-center hemodialysis is the most utilized form of dialysis treatment for Americans with end stage renal disease. With in-center hemodialysis a patient goes to a dialysis center where a staff of nurses and technicians administer treatment. Generally, in-center hemodialysis occurs three days a week for between three to five hours per session. During dialysis treatment the blood is removed from the body via an access (fistula, graft or catheter), filtered through an artificial kidney (dialyzer) and returned back to the body through the access. This blood is filtered many times during treatment to remove waste and maintain the chemical balance in the body. A nephrologist will prescribe the treatment and determine how long it will last. In addition to cleaning the blood, during dialysis treatment patients often will receive intravenous medications, such as erythropoietin (epogen) and iron, if necessary, to correct anemia and and a vitamin D sterol (zemplar, calcitriol, or hectoral).
Because healthy kidneys function 24 hours, seven days a week, and dialysis sessions are only for a few hours, three times a week, toxins build up in the body between treatments. Therefore, people on hemodialysis work with a dietitian and are recommended to limit or avoid foods high in phosphorus, potassium and sodium to feel their best between treatments. In addition, since most people with kidney failure have decreased urine output, there are fluid and salt restrictions. Dialysis patients are advised how much fluid to drink per day and what to eat by their dietitian based on their monthly lab reports and physical assessments.
The diet and fluid restrictions are necessary to avoid swelling and dangerous toxins from building up. The painful needle sticks are sometimes scary to some patients. A local anesthetic, such as lidocaine, can be used to help dull the pain, but that also requires a needle stick. There are also topical medications that will decrease the sensation of the needle stick. Some patients also report being embarrassed by the sight of their fistula and prefer to wear long sleeves.
Many hemodialysis centers have multiple shifts to accommodate their patients’ lifestyles. For patients who work, they can go to an early or late shift depending on their work or personal schedules. There are some hemodialysis centers that offer nocturnal dialysis, where a patient can come receive treatment overnight.
Pros and cons of in-center hemodialysis
Pros
- Trained medical professionals administer care
- No need to self-cannulate (insert needles oneself)
- No need to set up dialysis machine
- Sense of community
- Interact with other dialysis patients
- Regular contact with medical caregivers
Cons
- Need to take time to go to dialysis center
- Need to arrange for transportation to and from center
- Not much flexibility with scheduling treatments
- Dietary and Fluid restrictions to avoid swelling and toxin build up.
- Two needle sticks every treatment.
Hemodialysis access options
In order to perform hemodialysis an access must be created that allows blood to flow out of the body to be filtered and then be put back in. There are three access types:
The preferred type of access is the fistula. A National Vascular Access Improvement Initiative called Fistula First was established by the Centers for Medicare and Medicaid (CMS) along with companies providing dialysis and other members of the renal community to educate patients about the benefits of a fistula based on K/DOQI recommendations. The fistula is surgically created by attaching an artery and vein, usually inside the forearm. It generally takes a couple of months for a fistula to mature—allowing the vein to grow larger and stronger to accommodate dialysis. Fistulas are less likely to form blood clots or become infected, and historically last longer than the other access types
A graft is surgically created by connecting an artery or vein to artificial tubing usually inside the forearm. It usually takes three to six weeks after placement for the graft to be ready to be used.
When using a graft or fistula for hemodialysis, two needles are inserted into the access; one to remove blood from the body and the other to put it back in. While the needle sticks can be painful, many patients report that the sting is only for a second, and after time they get used to it. In addition, a technique called the buttonhole can be used with a fistula. With the buttonhole technique the exact same puncture site is used for every hemodialysis treatment. By using the same puncture site, and holding the needle at the same angle, over time scar tissue develops making it easier and less painful to stick the access.
Whether a patient will have a catheter, graft or fistula will be determined by their nephrologist after a thorough examination.
A catheter is immediately available for use but should only be used for a short period of time or in emergency cases whereas a graft and fistula need time to be surgically created, heal and mature. For patients who don’t have advance notice that they will need dialysis, a catheter is placed in a vein in the neck, chest or groin so they can receive treatment immediately. Tubes are attached to the catheter; one that lets the blood flow out of the body and a separate one to let the blood back in. With a catheter there is a greater chance of infection and blood flow is not optimal, therefore, groups such as the National Kidney Foundation (NKF) (in their Kidney Disease Outcome Quality Initiative (K/DOQI) guidelines), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and many nephrologists recommend a graft or fistula be used as a permanent access for patients who are able to support a vascular access.