In the wake of recent action by CMS to maintain Medicare Advantage funding, the time is ripe to follow up on a recommendation made by the Medicare Payment Advisory Commission 14 years ago: repeal the law prohibiting dialysis patients from enrolling in Medicare Advantage. The exclusion of end-stage renal disease (ESRD) patients from Part C deprives them of the opportunity to access two important benefits: care coordination by a single, accountable entity; and maximum out-of-pocket limitations.
ESRD Patients Lack Access to Care Coordination, Resulting in Avoidable Complications
As AHIP noted in a 2010 white paper, “health plans provide a life line” to patients with chronic conditions who are “at high risk of complications and medical emergencies.” MA plans can deploy “case managers—who are typically nurses—[to] contact patients to assess their needs, help them set health goals, and provide extensive, ongoing support.” Ironically, while ESRD epitomizes the high-risk, chronic condition, most newly diagnosed ESRD patients cannot access these care coordination services, which are not reimbursed in fee-for-service
(FFS) Medicare.
- CMS’ ESRD Disease Management Demonstration has shown that ESRD patients experience better outcomes when care management interventions are employed. Two successful demonstration sites have continued as Special Needs Plans, but those sites are available to only a fraction of ESRD patients. While the CMS Innovation Center has announced an accountable care organization model for ESRD patients, that project will also serve relatively few patients. The quickest avenue to scaling up care coordination for ESRD beneficiaries is through Part C.
- While there is no data available to confirm this, numerous anecdotal reports indicate that dialysis patients who were enrolled in MA prior to kidney failure and who have remained in their plans achieve better outcomes due to the care management provided by insurers.
- Results from the ESRD Disease Management Demonstration also indicate the possibility of savings for the Medicare program. At one site, by year three, hospitalization costs were reduced by 18 percent and overall expenditures by 11 percent.
- Accountability for the costs of avoidable complications is clouded by the fragmented nature of fee-for-service Medicare, and no provider has a financial incentive to prevent hospitalizations.
ESRD Patients Are Denied Access To Medicare Advantage’s Out-of-Pocket Limits
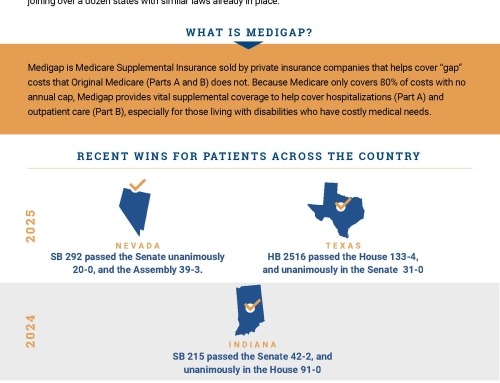
Part C has historically been favored by lower-income beneficiaries who cannot afford Medigap supplemental insurance. Since Medigap is not universally available to ESRD patients under 65, Part C could be an opportunity for ESRD patients to limit their out-of-pocket costs.
- MA plans have maximum out-of-pocket limits of $6,700, and most limit cost-sharing to $5,000 or less. Dialysis patients, restricted to fee-for-service Medicare, are over-represented in the top decile of out-of-pocket spenders—23 percent of them spend more than $8,235 per year—and can face cost-sharing of as much as $15,000.
- While there are always concerns that health plans might be less welcoming of sicker and potentially more costly enrollees, such fears have abated with regard to ESRD patients. Plans are not permitted to impose cost sharing for dialysis that exceeds that of FFS Medicare. Moreover, MedPAC found that three-fourths of enrollees who selected plans before their kidneys failed and remained in those plans afterward are in plans that charge no co-payment or coinsurance for dialysis.
- Because there is minimal cost-sharing permitted in Medicaid, ESRD patients have a perverse financial incentive to stop working and spend down their assets to become dually eligible.